Physician Guide to Spine Load and Fall Risk Management
Here is a quick screening guide for physicians to use during an office visit to determine if a patient with bone loss needs further intervention to reduce spine load and fall risk
|
|
|
|
|











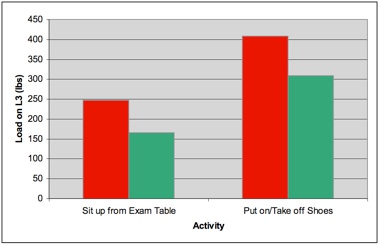
VERTEBRAL FRACTURE AND SPINE LOAD: Elevated spine loads occur throughout daily living. Excessive and repetitive spine loading have been shown to be associated with fracture in patients with osteoporosis (1-3).
-
•Evaluate your patient for excessive spine load. Watch your patient move while in the exam room. Spine loads are elevated during exam room activities such sitting up from an exam table or removing shoes.
-
•If you observe or learn that your patient with bone loss is engaging in repetitive and or elevated spine loading activities, refer them to rehabilitation to learn how to modify their activities to lower load on the spine.
-
1.Briggs AM, Wrigley TV, van Dieën JH, et al. The effect of osteoporotic vertebral fracture on predicted spinal loads in vivo. Eur Spine J. 2006;15(12):1785-95.
-
2.Hayes WC, Piazza SJ, Zysset PK. Biomechanics of fracture risk prediction of the hip and spine by quantitative computed tomography. Radiol Clin North Am. 1991;29(1):1-18.
-
3.Myers ER, Wilson SE. Biomechanics of osteoporosis and vertebral fracture. Spine. 1997;22(24 Suppl):25S-31S.
-
4.Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52(7):1121-9.
-
5.Yamada T, Demura S. Relationships between ground reaction force parameters during a sit-to-stand movement and physical activity and falling risk of the elderly and a comparison of the movement characteristics between the young and the elderly. Arch Gerontol Geriatr. 48(1):73-7.
-
6.Black DM, Steinbuch M, Palermo L, et al. An assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int. 2001;12(7):519-28.
-
7.Perkins BA, Olaleye D, Zinman B, Bril V. Simple Screening Tests for Peripheral Neuropathy in the Diabetes Clinic. Diabetes Care. 2001;24(2):250-256.
-
8.Hansson EE, Månsson N, Ringsberg KA, Håkansson A. Falls among dizzy patients in primary healthcare: an intervention study with control group. Int J Rehabil Res. 2008;31(1):51-7.
-
9.Kulmala J, Viljanen A, Sipilä S, et al. Poor vision accompanied with other sensory impairments as a predictor of falls in older women. Age Ageing. 2009;38(2):162-7.
-
10.Peterka RJ. Sensorimotor integration in human postural control. J Neurophysiol. 2002;88(3):1097-118.
-
11.Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction of balance. Suggestion from the field. Phys Ther. 1986;66(10):1548-50.
Copyright 2012 IONmed Systems
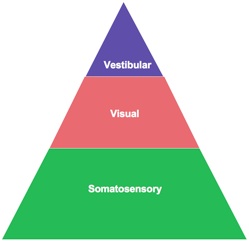
FALL RISK AND SENSORY LOSS: Evaluate the sensory component of balance. Peripheral nerve impairment and inner ear disorders can cause unsteadiness and dizziness that can lead to a fall (7-11).
-
•Conduct a pin-prick test on soles of feet to screen a patient for peripheral nerve loss (7).
-
•Ask your patient if they have vision loss or have been experiencing dizziness (8-9).
-
•Observe performance on a Romberg and foam test in your office (10-11).
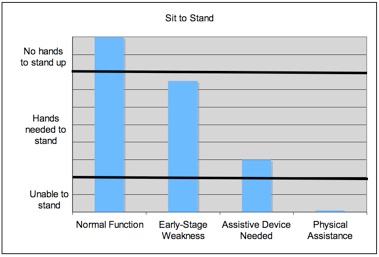
FALL RISK AND STRENGTH: Sit to stand performance has been linked to increased fall and fracture risk (4-6).
-
•Evaluate the strength component of balance. Ask your patient to stand up from a chair - if possible, with the use of their hands. (click here for more details)
